IN MY EXPERIENCE, precious few Americans recognize the variety and depth of policies included in the Affordable Care Act. Over the past several months, we have seen numerous report cards and other evaluations of the ACA on the occasion of its 5th anniversary. To communicate the law’s diversity, I offer an alternative five-year report card that grades the law by evaluating the success or failure of each of its 10 titles. Here’s my summary, based on assessing how each title has been implemented, followed by detailed discussion:
| Title | Name | Purpose | Grade |
| 1 | Quality Affordable Coverage for all Americans | Reform and expansion of private health insurance | A- |
| 2 | The Role of Public Programs | Medicaid expansion and reform | B+ |
| 3 | Improving the Quality and Efficiency of Health Care | Medicare and Delivery System Reform | A- |
| 4 | Prevention of Chronic Disease and Improving Public Health | Prevention, Wellness, and Public Health | B- |
| 5 | Health Care Workforce | Improving quality and quantity | C+ |
| 6 | Transparency and Program Integrity | Fraud and abuse control; clinical comparative effectiveness, transparency, and more | A- |
| 7 | Improving Access to Innovative Medical Therapies | Allowing biosimilar biopharmaceutical drugs in the US market | A- |
| 8 | Community Living Assistance Service & Supports | Cash assistance for temporarily or permanently disabled Americans | F |
| 9 | Revenue Provisions | Financing about half the cost of the full ACA | A |
| 10 | Strengthening Quality Affordable Health Care for All | Amendments to titles 1-9 | n/a |
Overall Grade – A-
Let’s consider each Title, one by one:
Title 1 is where the most controversial and well-recognized parts of the law reside: insurance market reforms such as eliminating pre-existing condition exclusions and medical underwriting, premium and cost sharing tax credits/subsidies to purchase private insurance through the public Exchanges/Marketplaces, the individual and employer mandates, and much more. After a horrible start with the healthcare.gov website disaster in the fall of 2013, federal officials got the system on track and provided coverage by this spring to about 11.7 million Americans, about 8 million of whom were previously uninsured.
Because of Title 1, the notion of the health insurance exchange has become embedded successfully in our health system’s infrastructure (including a proliferation of private health exchanges) as the nation moves — smartly or dumbly — toward health insurance as a retail/individual purchase market. The risk pool of enrollees is sufficiently balanced with participation from younger and healthier populations. Private health insurance premiums have not skyrocketed — indeed, private health insurance costs have stabilized over five years at a level unexpected by ACA supporters or critics. Because of this, federal ACA implementation costs have come in substantially below 2010 Congressional Budget Office projections. Exchange enrollment has been robust even in the most ACA-intransigent states such as Texas and Mississippi. The establishment of minimum essential benefits to nearly all privately insured Americans has triggered huge benefits for those in need of mental health and substance abuse services, for women consumers, and for those who had flimsy policies. Despite expectations of yet another disaster, the first round of individual mandate enforcement by the IRS during this just-completed tax filing season happened with remarkable lack of controversy.
Key concerns are that the subsidies are inadequate for millions of economically vulnerable Americans, and that cost sharing and narrow network requirements are discouraging many newly insured enrollees from accessing needed medical care (cost sharing such as deductibles have been rising significantly for 15 years in the US and the ACA established the first set of upper limits on this). There are future concerns about the financial sustainability of the state exchanges, the impact of the end of reinsurance and risk corridors after 2016, and the looming judgment in the King v. Burwell lawsuit. Nonetheless, it’s been a pretty remarkable performance looking back over five years. Grade: A-.
Title 2 is all about Medicaid, and especially the law’s expansion of Medicaid to all citizens with incomes under 138 percent of the federal poverty line (about $15,000 in annual income for a single adult) in all states beginning January 1, 2014. Because of the 2012 US Supreme Court decision in NFIB v. Sebelius, this expansion was made into an option rather than a requirement for all states.
As of today, 30 states (including Washington, DC) have expanded and 21 have not, with four currently in active consideration. Since the fall of 2013, about 11.7 million have newly enrolled in Medicaid, and between 8-9 million are estimated by the US Department of Health & Human Services to have been uninsured prior to enrolling. Total enrollment in Medicaid and the Children’s Health Insurance Program is now estimated at over 70 million Americans. If all 50 states currently were participating in the expansion, we would see between 4-5 million more enrolled in Medicaid.

The expanding states have seen dramatic drops in levels of uncompensated medical care costs, more financially healthy hospitals, and more. One study showed a dramatic increase in diagnosis of diabetes in the expanding vs. the non-expanding states. If Title 2 had been implemented as written by Congress, the grade for this Title would most definitely be an A. It’s only a matter to time before all states join the expansion — my prediction is that all states will be participants by 2020 at the latest. Because of the US Supreme Court ruling, it’s Grade: B+.
Title 3 does two major chores. First, it changes Medicare to improve benefits for enrollees and reduces the rate of Medicare spending to finance about half the cost of the ACA’s coverage expansions in Titles 1 and 2. Second, it initiates a varied series of reforms, initiatives, and experiments aimed at improving the quality, efficiency, and effectiveness of medical care as delivered in the US. Let’s look at these in turn.
First, the Medicare beneficiary improvements — wellness visits, no cost sharing for preventive services, closing the prescription drug coverage gap (aka the donut hole) — all happened without controversy. The payment reductions to hospitals, home health, hospice, and other providers are happening as anticipated. And though adjustments have been made to significant reductions in payments to Medicare Advantage (Part C) insurance plans, the payment disparity between these plans and the fee-for-service payments through Medicare Parts A & B has been substantially and successfully reduced. Incessant Republican accusations that Obamacare would destroy Medicare and Medicare Advantage have proven hollow.
Second, the delivery system reforms, slowly and surely, are showing positive results. Approximately 700 “accountable care organizations” have been established in Medicare (with accompanying ACOs on the private side), and recent data on the “pioneer” ACOs shows some significant achievers on both cost and quality. Readmissions of Medicare patients within 30 days after discharge have begun to decline significantly (160,00 fewer in 2013). Hospital acquired conditions (infections, falls, and other serious mishaps) have dropped significantly since 2010, saving an estimated 50,000 lives. More broadly, the movement of US health care financing away from fee-for-service and toward paying-for-value is happening and accelerating.
The results are more impressive than any supporters believed possible in 2010. Still, it’s a slow and steady climb and many results are too preliminary for long term judgments. But, here’s a dead giveaway about Title 3. Republican Sens. Orrin Hatch of Utah and Richard Burr of North Carolina, and Rep. Fred Upton, Republican of Michigan, are the influential lead sponsors of the Patient CARE Act advanced in both 2014 and 2015 as a Republican replacement for the ACA. Indeed, the legislation would repeal the entire ACA — with one fat and juicy exception — it leaves Title 3 totally intact! Grade: A-.
Title 4 is all about prevention, wellness, and public health. I love this title and it breaks my heart. The Title established a new national Prevention and Public Health Fund with $18.25 billion dedicated between 2010 and 2022, with $2 billion per year after that. But Congress cut $6.25 billion between 2013-21, and a large share of the remainder has been diverted to supplant funding lost from the budget sequestration process that took effect in 2013.
The title also directed the creation of a National Prevention Strategy that was released by then US Surgeon General Regina Benjamin in 2011, a terrific document that has received almost no attention or effective implementation since its launch. Here’s hoping that the new surgeon general, Dr. Vivek Murthy, can breathe some life into the National Prevention Strategy and the National Prevention Council, also established under Title 4.
Meanwhile, calorie labeling in chain restaurants was supposed to happen within two years of the law’s signing. After an immense food fight over proposed regulations issued by the US Food and Drug Administration over such issues as listing calories by the pizza slice or pie and whether to include movie theater popcorn, labeling will be required by December 1, 2015. Too long a time coming.
We could be doing so much more and so much better, and my grade: B-.
Title 5 is all about the health care workforce. The crown jewel of this title was the establishment of a National Health Care Workforce Commission, the first ever, to provide comprehensive and unbiased information to Congress, the administration and states on how to align federal resources with national health care workforce needs. The Comptroller General of the GAO was directed to nominate the commission members and did so in the fall of 2010, appointing a talented and exceptional group of workforce experts. Four-and-a-half years later, the commission has never met, and the terms of office of all appointees have expired. Why? Because the Republican-controlled House of Representatives refused to appropriate the $2 million needed to finance the Commission because it was established as part of “Obamacare.” What a tragedy and missed opportunity!
Meanwhile, a large new infusion of $12.5 billion in funding for community health centers and the National Health Service Corps actually happened — mostly. Congress swiped back $3 billion of it in one of the budget cutting exercises. Happily, the recently approved Medicare physician payment law includes another two years of funding for both. Community health centers and the NHSC are thriving — thanks to the ACA. Grade: C+.
Title 6 is what I call the “grab bag.” It’s where Congress placed items it wanted in the law that did not fit into any of the more coherent other titles. Let’s explore the bigger ones in turn (I’ll grade each items pass/fail):
The Physician Payment Sunshine Act requires all manufacturers of drugs, medical devices, biologics, and supplies to report all gifts and other transfers of value made to physicians and teaching hospitals for publication on a federal website. The reporting, now called Open Payments on the website of the Centers for Medicare and Medicaid Services (CMS), was launched last fall, behind schedule. The data collection and reporting both need improvement and both will happen. Pass.
The Patient Centers Outcomes Research Institute (PCORI), established in Title 6, was launched in 2011 and has initiated a robust research agenda on clinical comparative effectiveness. PCORI has infused $868 million in new research dollars that helped the research community absorb other cuts to the National Institutes of Health (NIH). Some criticize PCORI’s priorities and lack of headline grabbing results, but it’s up and running. Pass.
Deterring Medicare and Medicaid fraud and abuse is the most important element of Title 6. Partly with the help of these provisions, as well as an energetic focus on stopping fraud and abuse, the first six years of the Obama presidency have been the most successful ever in combating and deterring those who want to steal money from these programs. Importantly, the focus has shifted from chasing bad guys with sacks of cash to preventing bad guys from stealing in the first place. Lots of encouraging progress. High Pass.
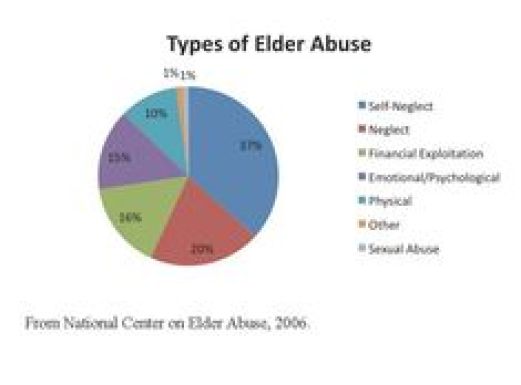 The Elder Justice Act, a bipartisan effort to upgrade and coordinate national and state efforts to combat physical abuse, neglect, and financial exploitation of senior citizens represented the achievement of a decade’s work, a milestone for Republicans and Democrats. And, Congress never appropriated the money to realize the act’s ambitions, and the ACA’s authorization period has expired. Big Fail.
The Elder Justice Act, a bipartisan effort to upgrade and coordinate national and state efforts to combat physical abuse, neglect, and financial exploitation of senior citizens represented the achievement of a decade’s work, a milestone for Republicans and Democrats. And, Congress never appropriated the money to realize the act’s ambitions, and the ACA’s authorization period has expired. Big Fail.
Overall Title 6 Grade: A-.
Title 7, for the first time, authorizes the US FDA to approve the manufacture, marketing, and sale of so-called “biosimilar products” in the US pharmaceutical market. Biosimilars are generic-like versions of biopharmaceutical drugs, the major growth area of the global pharmaceutical industry. The 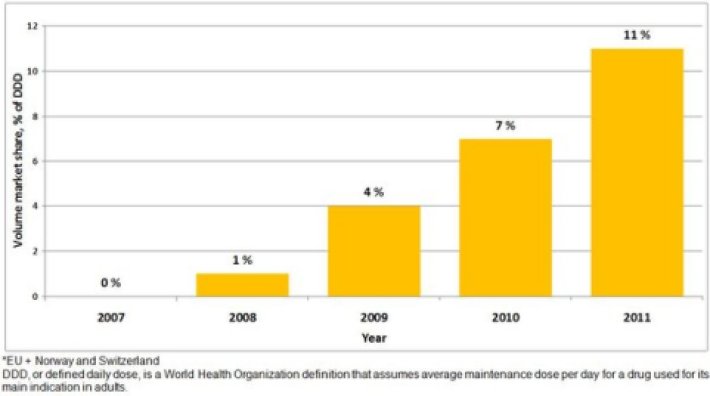 European Union, Japan, Brazil, and many other nations permitted biosimilars before the ACA opened the door in the US. So we are playing catch up. Both Democrats and Republicans strongly supported this during the ACA legislative process — with disagreements over how many years drug makers could keep their data secret. Big pharma and biotech wanted at least 12 years of data exclusivity, and almost everyone else — business, labor, consumers, insurers, providers — wanted no more than five years. The final number was 12!
European Union, Japan, Brazil, and many other nations permitted biosimilars before the ACA opened the door in the US. So we are playing catch up. Both Democrats and Republicans strongly supported this during the ACA legislative process — with disagreements over how many years drug makers could keep their data secret. Big pharma and biotech wanted at least 12 years of data exclusivity, and almost everyone else — business, labor, consumers, insurers, providers — wanted no more than five years. The final number was 12!
Just this past March, the FDA approved the first biosimilar for the US market, a Novartis copycat of an Amgen cancer treatment. Amgen is fighting in court, of course. Biosimilars will become an important and growing part of the US pharma market in the next decade. While FDA is starting to approve these new agents, they have yet to issue regulations to guide the process, so let’s knock this grade down a mark. Grade: A-.
Title 8, Community Living Assistance Services and Supports (CLASS) was the personal priority of my late boss, Sen. Edward Kennedy, who wanted to create a new way for Americans who are temporarily or permanently disabled to get cash support to enable them to live independently in the community. The design of Title 8 was flawed in serious ways. Bottom line is that it’s perilously hard to establish a voluntary insurance program anywhere, and especially in long term care — and a mandate on top of Title 1’s individual mandate was inconceivable politically. Rather than fix these flaws, which some thought feasible, Congress and President Obama repealed Title 8 in toto in legislation signed in January 2013. America needs to figure out a better way to help Americans with disabilities. Grade: F.
Title 9 includes provisions that raise certain taxes or otherwise offset federal costs to finance about half the cost of the entire ACA, especially the coverage portions of Titles 1 and 2. This is where you will find:
- New Medicare taxes on earned and unearned income for individuals and families making more than $200,000 or $250,000 per year;
- The so-called “Cadillac Tax,” a 40 percent excise tax on expensive health plans. The tax takes effect in 2018, though insurers and employers have been getting ready for years by reducing the cost of their plans;
- New taxes and fees on pharmaceutical makers, medical device manufacturers, and health insurance companies.
- A lot more, including my favorite, a 10 percent excise tax on indoor tanning services (substituted at the last minute for a proposed tax on elective cosmetic surgery) that was dubbed the “bo-tax.”
Lots of ongoing controversy has erupted over several of these, especially the medical device, the “Cadillac,” and the health insurance taxes — all subject to aggressive repeal campaigns. The weakness of the repeal campaigns is how to replace lost revenues or savings.
The big Kahuna in this title is the new Medicare tax — accounting for about half the title’s total revenue. Had the ACA been bipartisan, there’s no way this would have survived the legislative process, especially the taxes on unearned income — a dream for Democrats and a nightmare for Republicans. If you ask me why the Koch brothers, David and Charles, despise Obamacare so much, I point to ACA section 9015.
As we saw in the recent Medicare physician payment legislation approved by Congress last month, it’s always easier to pass legislation when you don’t have to pay for it! In that recent bill, Congress and President Obama lathered $140 billion onto the federal debt and never would have passed it but for Republicans and Democrats closing their eyes, joining hands, and passing the tab onto our children and grandchildren.
So, no matter how much you may despise any or all of these Title 9 provisions, let’s show a patina, a dab, of respect for the Democrats in Congress who passed comprehensive national health reform and had the integrity and guts to pay for it. So David and Charles, take note: Grade: A.
Title 10 is the law’s aardvark. Because of the unprecedented political controversy during the ACA  legislative process, it was impossible for Democrats, as the legislation proceeded through the Senate, to add amendments by substituting a new draft. The only way to get to win was for Democrats to add their final amendments to the bill in a single separate title knows as Title 10, sometimes called the “Manager’s Amendment” (the manager being then-Senate Majority Leader Harry Reid).
legislative process, it was impossible for Democrats, as the legislation proceeded through the Senate, to add amendments by substituting a new draft. The only way to get to win was for Democrats to add their final amendments to the bill in a single separate title knows as Title 10, sometimes called the “Manager’s Amendment” (the manager being then-Senate Majority Leader Harry Reid).
Team Obama refers to Title 10 as the Indian Health Care Improvement Act, and it’s true this is the largest element of a title chock full of them. So let’s dispense with a grade for this one.
My summary grade for the ACA at five years: A-. An alternative grade would be “incomplete.” Any law of the scope and magnitude of the ACA is a work in progress that never ends. If the 1935 Social Security Act or the 1965 law creating Medicare and Medicaid had never changed since their signings by Presidents Roosevelt and Johnson, respectively, we’d judge them failures today — good for their times, and inadequate for today’s society and needs.
So it is with the ACA. The law’s signing in March 2010 by President Obama was the end of a long struggle to pass some form of comprehensive health reform. Also, it is only the beginning of a new period and process to fix, improve, adjust, and modernize the ACA to fit the always-changing needs of our dynamic society. Thus far, I contend that the ACA stands the test of time, though not forever. That’s up to the next generations, up to my students, up to all of us and all of you.
John E. McDonough teaches at the Harvard TH Chan School of Public Health and is the author of Inside National Health Reform.
CommonWealth Voices is sponsored by The Boston Foundation.
The Boston Foundation is deeply committed to civic leadership, and essential to our work is the exchange of informed opinions. We are proud to partner on a platform that engages such a broad range of demographic and ideological viewpoints.
